
US flu activity climbs, with more deaths in kids
The nation’s flu activity continued a steady rise last week, with 44 states at the high or very high level and that national test positivity just shy of 30%, the Centers for Disease Control and Prevention (CDC) said today in its weekly update.
Outpatient visits for flulike illness have been above the national baseline for 9 weeks in a row. Of samples that tested positive for flu at public health labs, nearly all were influenza A, and subtyped influenza A samples were about evenly split between the H3N2 and 2009 H1N1 strains.
:max_bytes(150000):strip_icc()/Health-GettyImages-1481613605-f1a3ef6060494e1d9cd3a68a02bdfdde.jpg)
On the CDC’s flu activity map, most of the country is awash in shades of red that reflect high or very high activity. However, some states are shaded purple, the highest level on the activity scale. They include Southeastern states such as Louisiana, South Carolina, and Tennessee, but also several in the Northeast, including Massachusetts, New Jersey, New York, and New Hampshire.
16 more pediatric flu deaths
The CDC reported 16 more pediatric flu deaths, which push the season’s total to 47. The deaths occurred between the middle of December and the week ending January 25. All involved influenza A, and, of 13 subtyped samples, 7 were H1N1 and 6 were H3N2.
For deaths overall, the level remained steady, with flu making up 1.6% of all deaths last week.

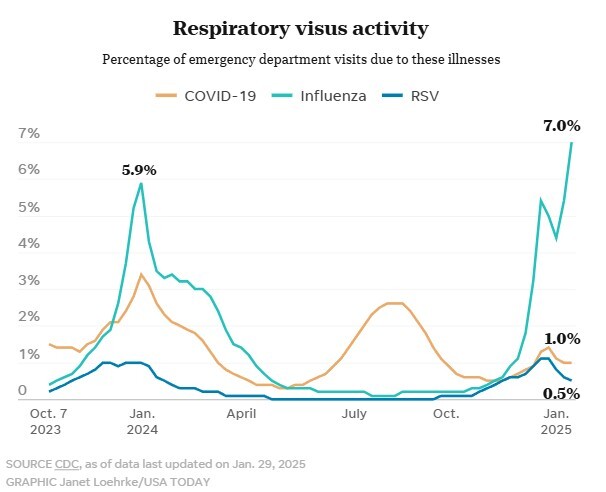
Emergency department (ED) visits for flu are at the very high level and are increasing in all age-groups, making up 7% of all ED visits, the CDC said in its weekly respiratory virus snapshot. Meanwhile, hospitalizations for flu remain elevated and are likewise on the rise for all age-groups.
COVID holds steady; RSV ebbs
Though COVID-19 wastewater detections moved from the medium back into the high category last week, ED visits are still low, highest in young children and elevated in older people. Meanwhile, hospitalizations for the virus remain elevated and are highest in seniors. Deaths from COVID trended downward but still make up 1.6% of all deaths in the United States.

Wastewater levels were up a bit in all regions and are still highest in the Midwest. The CDC said activity is likely growing or growing in the Southeast and West, along with parts of the northeast.
Test positivity for COVID held steady, at 5.4%
For respiratory syncytial virus (RSV), which has been a notable contributor to respiratory virus activity this season, showed downward trends, with ED visits—highest in children– and wastewater detections at the moderate level. Hospitalizations are also highest for children, though levels are elevated among older people in some parts of the country.
Is a ‘quademic’ swirling? What you should know about flu, RSV, COVID and norovirus

A nationwide surge in flu, COVID-19, RSV and norovirus infections is fueling concerns of a possible virus “quademic.” Or is it just winter?
The three respiratory viruses plus norovirus, a gastrointestinal virus, are the “main players in our winter virus pantheon,” said Dr. Thomas Russo, who heads the infectious diseases department at the University at Buffalo School of Medicine. Russo added that they can circulate at other times of year but tend to peak in winter.
“Do we have a lot of cases? The answer is yes,” Russo told USA TODAY. “The ’emic’ part of it is a bit of a gimmick, but we do have these viruses circulating and causing infections right now.”

All are not peaking at precisely the same time, but spikes in the viruses are “clustering,” said Dr. Ogbonnaya Omenka, director of equitable population health for Humana Indiana Pathways.
“The term (quademic) does not imply a public health doomsday,” Omenka said. “We deal with them every year.”
A Centers for Disease Control and Prevention flu report for the week of Jan. 25 showed almost 30% of lab tests for flu were positive and the rate was trending higher. There were also 16 deaths related to influenza, bringing the total to 47 deaths this season, according to the report.

RSV numbers appear to have peaked in recent weeks and are dropping. COVID-19 was at a 5.4% test positivity for the week that ended Jan. 25, and 1.6% of all deaths in the U.S. that week were linked to the virus, per CDC data. Russo said COVID-19 numbers appear to be “smoldering” and he expects them to peak in the coming weeks.
“We haven’t seen the (COVID) peak we have seen in previous winters,” Russo said. “Peaks in RSV and influenza have been greater, and we may see a peak in COVID in upcoming weeks.”
Health departments are not required to report norovirus cases to the CDC, but Russo says it’s been a “big norovirus year.” COVID and norovirus are a problem all year round, although they tend to peak in winter months when people are enclosed indoors in close spaces, he said.

Symptoms can be similar
Russo said it is unlikely that someone would get two of the infections at the same time, and that “to get all four is certainly unlikely, particularly if you are vaccinated.” Symptoms can be similar and can include fever, chills, cough, sore throat, runny nose, muscle or body aches, fatigue, headache, vomiting and diarrhea.
Because the viruses share some common characteristics, including symptoms, test results are the only way to know exactly the type of virus involved in each case. But it also means that preventing one may also help prevent all of them, Omenka said. Vaccines are available for the flu, COVID and RSV, and Russo and Omenka say vaccinations could be crucial.
Vaccination is key to avoiding infection, minimizing illness
“It is important for people to realize that these vaccines are critical for preventing infection,” Russo said.
He said the vaccines are imperfect and some people will get infected anyway, but that even then the vaccine can lessen the severity of the disease. Vaccines also help keep people from spreading the disease. He described vaccines as “probably the greatest medical invention in terms of saving lives and minimizing years of life lost.” A huge body of research shows the rewards outweigh the risk, which is “very low but not zero,” he said.

“You hear ‘My neighbor got the vaccine and got sick,'” Russo said. “Yes, but they probably had a much less serious case.”
Viruses can mutate, and immunization from a long-ago vaccination or from having experienced the disease can wane over time.
“We must keep in mind the arms-race aspect of dealing with infectious outbreaks, which results in playing catch-up with the threat,” Omenka said.

RSV can be confused with other viruses
RSV, respiratory syncytial virus, usually peaks in December and January while infecting the nose, throat and lungs, usually causing mild, cold-like symptoms, the CDC says. Those symptoms make it difficult to distinguish it from the common cold, COVID-19, or influenza.
“And there’s a ton of flu around right now,” Russo said.
Almost every child is infected in the first five years of life − and it is the most dangerous in the first year of life. It also can be dangerous for the elderly and those who are immunocompromised.
:max_bytes(150000):strip_icc()/flu-GettyImages-1421116841-bba3baea56c74a19b232b7f5d3306ccc.jpg)
Parents are ‘low-hanging fruit’ for norovirus spread
Norovirus causes inflammation of the stomach and intestines and is known as stomach flu. It is highly contagious, can survive and thrive on surfaces and can’t be killed with most disinfectant sprays, he said. Russo suggested cleaning surfaces with diluted bleach and washing clothes in hot water to curb contamination.
“Imagine a household with young children where one of the children gets norovirus at day care or school,” Russo said. “Mom and dad are taking care of the child − and become low-hanging fruit for infection. It can rip through households.”
Cruise ships and other places where people are in close quarters can lead to an outbreak, he said.
“Dehydration can be a serious problem, and there can be 24-48 hours of fever, vomiting, diarrhea and generally short-term, total misery,” he said. He suggested drinks with electrolytes as opposed to simply water while trying to weather the norovirus storm.
Human case of avian flu detected in England
UKHSA confirms rare case of bird flu A(H5N1) in the West Midlands region.

UKHSA has confirmed a case of influenza A(H5N1) in a person in the West Midlands region. Bird-to-human transmission of avian influenza is rare and has previously occurred a small number of times in the UK.
The person acquired the infection on a farm, where they had close and prolonged contact with a large number of infected birds. The risk to the wider public continues to be very low.
The individual is currently well and was admitted to a High Consequence Infectious Disease (HCID) unit.
The birds were infected with the DI.2 genotype, one of the viruses known to be circulating in birds in the UK this season. This is different to strains circulating among mammals and birds in the US.

Although there has been no demonstrated human-to-human transmission despite extensive recent surveillance of influenza A(H5N1), UKHSA has been tracing all individuals who have been in contact with the confirmed case of avian influenza. Those at highest risk of exposure have been offered antiviral treatment. This is done to reduce the chance that any virus they have been exposed to will be able to cause infection.
The case was detected after the Animal and Plant Health Agency (APHA) identified an outbreak of avian influenza A(H5N1) in a flock of birds. UKHSA carried out routine monitoring on people who had been in close contact with the infected birds.

Professor Susan Hopkins, Chief Medical Adviser at UKHSA, said:
The risk of avian flu to the general public remains very low despite this confirmed case. We have robust systems in place to detect cases early and take necessary action, as we know that spillover infections from birds to humans may occur.
Currently there is no evidence of onwards transmission from this case.
People are reminded not to touch sick or dead birds and it’s important that they follow Defra advice about reporting any suspected avian influenza cases.

UK Chief Veterinary Officer Christine Middlemiss said:
While avian influenza is highly contagious in birds, this is a very rare event and is very specific to the circumstances on this premises.
We took swift action to limit the spread of the disease at the site in question, all infected birds are being humanely culled, and cleansing and disinfection of the premises will be undertaken all to strict biosecure standards. This is a reminder that stringent biosecurity is essential when keeping animals.
We are seeing a growing number of avian flu cases in birds on both commercial farms and in backyard flocks across the country. Implementing scrupulous biosecurity measures will help protect the health and welfare of your birds from the threat of avian influenza and other diseases.
Andrew Gwynne, Minister for Public Health and Prevention, said:
The safety of the public is paramount, and we are monitoring this situation closely.
The risk of wider or onward transmission is very low, however the UK remains prepared and ready to respond to any current and future health threats.
We recently added the H5 vaccine, which protects against avian influenza, to our stockpile as part of our preparedness plans.
UKHSA will publish further details about the confirmed human case in due course.























:max_bytes(150000):strip_icc()/KateLead-7b680bfb11ee419895fc7f5dee2860a7.jpg?w=1200&resize=1200,0&ssl=1)










:max_bytes(150000):strip_icc():focal(999x0:1001x2)/catherine-ohara-013026-7-4b5b413a646d4f15a1fd15ac8b933811.jpg?w=1200&resize=1200,0&ssl=1)







